Product Overview
[Drug Name]
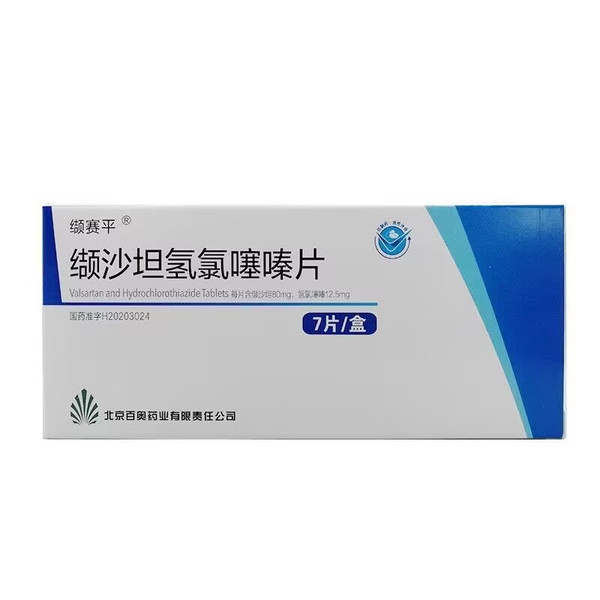
Generic Name: Valsartan Hydrochlorothiazide Tablets
Trade Name: Valsartan Hydrochlorothiazide Tablets (7 tablets)
[Main Ingredients]
This product is a combination preparation. Each tablet contains 80mg of valsartan and 12.5mg of hydrochlorothiazide.
[Properties]
This product is a film-coated tablet that appears white after removal of the coating.
[Indications/Main Functions]
It is used to treat mild to moderate essential hypertension where blood pressure cannot be adequately controlled with a single medication. This product is not suitable for the initial treatment of hypertension.
[Specifications]
7 tablets
[Dosage and Administration]
Each tablet contains 80 mg of valsartan and 12.5 mg of hydrochlorothiazide. If blood pressure cannot be adequately controlled with valsartan alone, or if 25 mg of hydrochlorothiazide once daily is insufficient, or if hypokalemia occurs, this tablet (containing 80 mg of valsartan/12.5 mg of hydrochlorothiazide) can be used once daily. Maximum antihypertensive effect is achieved within 2 to 4 weeks of treatment. Renal Impairment: For patients with mild to moderate renal impairment (glomerular filtration rate (GFR) ≥30 mL/min) does not require dose adjustment. There are no data on the use of this drug in patients with severe renal impairment (GFR <30 mL/min) or those on dialysis. When using diuretics in patients with severe renal impairment (GFR <30 mL/min), hydrochlorothiazide is the preferred choice, and therefore this drug is not recommended. Due to the presence of hydrochlorothiazide, this drug is contraindicated in patients with anuria (see [Contraindications]). Hepatic impairment: No dose adjustment is required in patients with mild to moderate hepatic impairment. There are no data on the use of salsartan in patients with severe hepatic impairment, and liver disease does not significantly alter the pharmacokinetics of salsartan. In patients with severe hepatic impairment, salsartan diuretics may cause electrolyte imbalances, hepatic encephalopathy, and hepatorenal syndrome; such patients should use salsartan diuretics with caution. This drug should be used with caution in patients with biliary obstructive disease or severe hepatic impairment (see [Precautions]).
[Adverse Reactions]
See package insert for details.
[Contraindications]
- Hypersensitivity to valsartan, hydrochlorothiazide, other sulfonamides, or any of the ingredients in this product.
- Pregnancy (see [Use in Pregnant and Lactating Women]).
- Biliary cirrhosis or cholestasis.
- Anuria.
- Concomitant use of angiotensin receptor blockers (ARBs) (including valsartan) or angiotensin-converting enzyme inhibitors (ACEIs) with aliskiren in patients with type 2 diabetes (see [Drug Interactions]).
[Precautions]
Caution is advised when administering this product with potassium-sparing diuretics, potassium supplements, potassium-containing salt substitutes, or other medications that increase potassium levels (e.g., heparin). Thiazide diuretics can induce new hypokalemia or worsen existing hypokalemia. Caution is advised when using thiazide diuretics in patients with severe potassium depletion (e.g., salt-losing nephropathy and prerenal (cardiogenic) renal impairment). If hypokalemia is accompanied by clinical signs (e.g., muscle weakness, paresis, or electrocardiographic changes), this product should be discontinued. It is recommended to correct hypokalemia or any concomitant hypomagnesemia before starting thiazide drugs, and blood potassium and magnesium concentrations should be checked regularly. All patients receiving thiazide diuretics should be monitored for electrolyte imbalances, especially blood potassium. Thiazide diuretics can induce new hyponatremia and hypoammonemic alkalosis or aggravate existing hyponatremia. Hyponatremia accompanied by neurological symptoms (nausea, progressive disorientation, apathy) has been observed in individual cases. Regular monitoring of blood sodium concentration is recommended. Patients with sodium and/or blood volume depletion In rare cases, symptomatic hypotension may occur when patients with severe sodium and/or blood volume depletion (e.g., high-dose diuretics) are started on this product. Hyponatremia and/or blood volume depletion should be corrected before starting treatment with this product. Otherwise, treatment should be closely monitored medically. If hypotension occurs, the patient should be placed in a supine position and normal saline may be administered if necessary. Treatment can be resumed after blood pressure stabilizes. Patients with renal artery stenosis Because blood urea and serum creatinine may increase, this drug should be used with caution in patients with unilateral or bilateral renal artery stenosis or isolated renal artery stenosis for the treatment of hypertension. Patients with renal impairment No dose adjustment is required for patients with mild to moderate renal impairment (glomerular filtration rate (GFR) ≥ 30 mL/min). There is no data on the use of this drug in patients with severe renal insufficiency (GFR less than 30 mL/min) or dialysis. In patients with severe renal impairment (GFR < 30 mL/min), a diuretic is preferred, so this product is not recommended. Due to the presence of hydrochlorothiazide, this product is contraindicated in patients with anuria (see [Contraindications]). Avoid the concomitant use of angiotensin receptor blockers (ARBs) (including valsartan) or angiotensin-converting enzyme inhibitors (ACEIs) with aliskiren in patients with severe renal impairment (GFR < 30 mL/min) (see [Drug Interactions]). Patients with hepatic impairment No dose adjustment is required for patients with mild to moderate hepatic impairment. There are no data on the use of valsartan in patients with severe hepatic insufficiency. Liver disease does not significantly alter the pharmacokinetics of hydrochlorothiazide. In patients with severe hepatic impairment, thiazide diuretics may cause Electrolyte imbalance, hepatic encephalopathy and hepatorenal syndrome, such patients should use thiazide diuretics with caution. This product should be used with caution in patients with biliary obstructive disease or severe liver damage (see [Dosage and Administration] and [Pharmacokinetics]). Angioedema Angioedema, including laryngeal and glottis edema, causing airway obstruction and/or swelling of the face, lips, pharynx, and/or tongue, has been reported in patients treated with valsartan; some of these patients have a history of angioedema with other drugs (including ACE inhibitors). Patients who develop angioedema should immediately discontinue this product and should not use it again. Systemic lupus erythematosus There have been reports that thiazide diuretics, including hydrochlorothiazide, can induce or aggravate systemic lupus erythematosus. Other metabolic disorders Thiazide diuretics, including hydrochlorothiazide, can Impairs glucose tolerance and increases serum cholesterol and triglyceride levels. Like other thiazide diuretics, hydrochlorothiazine can increase serum uric acid levels due to decreased uric acid clearance and may cause or worsen hyperuricemia in susceptible patients and trigger gout. Thiazides reduce urinary calcium excretion and may mildly increase serum calcium in the absence of known abnormalities of calcium metabolism. Because hydrochlorothiazine may increase serum calcium concentrations, caution should be exercised when used in patients with hypercalcemia. Significant hypercalcemia that is unresponsive to discontinuation of the thiazide or ≥12 mg/dL may indicate an underlying non-thiazide-dependent hypercalcemia. Parathyroid pathology has been observed in a small number of patients with hypercalcemia and hypophosphatemia who have received long-term thiazide therapy. Changes. If hypercalcemia occurs, further diagnosis is necessary. Systemic conditions Allergies and asthma patients are prone to allergic reactions to hydrochlorothiazide. Acute angle-closure glaucoma Hydrochlorothiazide (sulfonamide) can cause acute temporary myopia and atopic reactions of acute angle-closure glaucoma. Symptoms include acute onset of decreased visual acuity or eye pain and usually occur within a few hours to a few weeks after starting the medication. Untreated acute angle-closure glaucoma can lead to permanent blindness, and the main treatment is to stop hydrochlorothiazide as soon as possible. If intraocular pressure is still not controlled, immediate medical or surgical treatment needs to be considered. Risk factors for the development of acute angle-closure glaucoma may include a history of allergy to sulfonamides or penicillin. Patients with heart failure/post-myocardial infarction In patients whose renal function depends on the activity of the renin-angiotensin-aldosterone system (e.g., patients with severe congestive heart failure), treatment with ACE inhibitors or ARBs has been associated with oliguria and/or progressive azotemia, and rarely with acute renal failure and/or death. Evaluation of patients with heart failure or post-myocardial infarction after using this product should always include an assessment of renal function. Dual blockade of the renin-angiotensin system (RAS) Extreme caution should be exercised when angiotensin receptor blockers (ARBS), including esaltan, are used concomitantly with other drugs that block the renin-angiotensin system (RAS), such as angiotensin-converting enzyme inhibitors (ACEIs) or aliskiren (see [Drug Interactions]). Non-melanoma skin cancer is based on the Danish National Cancer Institute. Two epidemiological studies based on the National Health and Family Planning Commission (NHC) found that the risk of developing non-melanoma skin cancer (NMSC) (basal cell carcinoma (BCC) and squamous cell carcinoma (SC)) increased with increasing cumulative exposure to hydrochlorothiazide. Long-term use of hydrochlorothiazide may increase the risk of developing NMSC. Based on data from existing epidemiological studies, a dose-dependent relationship between NMSC and the cumulative dose of HCTZ has been observed. One study included a population consisting of 71,533 cases of BCC and 8,629 cases of SCC, along with 1,430,833 and 172,462 controls, respectively. The adjusted odds ratio (OR) for high-dose HCTZ (≥5,000 mg cumulative) for BCC was 1.29 (95% CI: 1.23-1.35) and the adjusted OR for C was 39 (95% CI: .6-1.6). A clear cumulative dose-relief relationship was observed when 8-431 was used to treat BCC and CC. Another study confirmed a possible association between lip cancer (SCC) and HCTZ exposure: a risk set sampling strategy was used to match 633 cases of lip cancer with 63,067 controls. The significant cumulative dose-relief relationship showed that the adjusted R21 (95%: 17-26 at the high dose level (approximately 2009) increased to R9 (30-49 at the highest cumulative dose of approximately 100) and increased to R77 (5.7-10.5). For example: a cumulative dose of 1000 mg is equivalent to a daily fixed dose of 25 mg, taken daily for more than 10 years. Photosensitivity reaction to hydrochlorothiazine is a possible pathogenesis of NMS. Patients taking hydrochlorothiazine should be informed of the risk of NMSC and Patients are advised to regularly inspect their skin for new lesions and promptly report any suspicious skin lesions. Patients should be advised to take possible preventive measures, such as limiting exposure to sunlight and taking adequate protection when in the sun, to minimize the risk of skin cancer. Suspicious skin lesions should be promptly examined, which may include histological examination of biopsies. Therefore, the use of hydrochlorothiazide in patients with a previous NMSC may need to be reconsidered (see [Adverse Reactions]). The effect on the ability to drive and operate machinery is similar to that of other antihypertensive drugs. Patients taking this drug should be cautious when waiting to drive or operating machinery. The effects on athletes include: This product, hydrochlorothiazide, and thiazide diuretics can affect the metabolism and excretion of stimulants, thereby potentially reducing the sensitivity of urine tests for stimulants. Therefore, athletes should use it with caution.