Product Overview
[Drug Name]
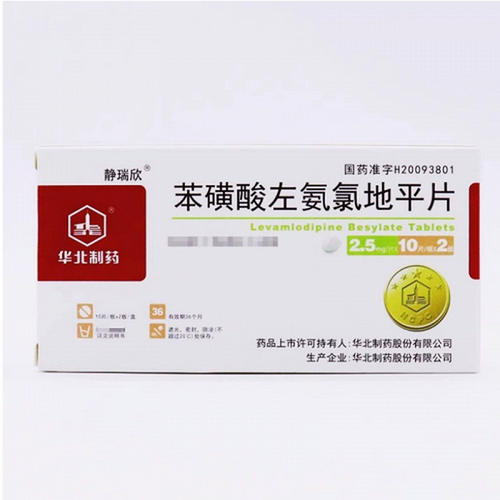
Generic Name: Levoamlodipine Besylate Tablets
Trade Name: North China Pharmaceutical Levoamlodipine Besylate Tablets 5mg x 14 Tablets
[Main Ingredient]
Levoamlodipine Besylate.
[Properties]
This product is white tablets.
[Indications/Main Functions]
1. Hypertension. 2. Angina pectoris.
[Specifications]
5mg x 14 tablets
[Dosage and Administration]
Oral: 1. The initial dose for the treatment of hypertension and angina pectoris is 2.5 mg once daily. The dose can be increased based on the patient's clinical response, up to a maximum of 5 mg once daily. 2. No dose adjustment is required when this product is used in combination with thiazide diuretics, beta-blockers, and angiotensin-converting enzyme inhibitors.
[Adverse Reactions]
This product is well tolerated within the 10 mg/day dose range, with most adverse reactions being mild to moderate. Discontinuation of this product due to adverse reactions occurred in only 1.5% of patients, which was not significantly different from placebo (approximately 1%).The most common adverse reactions were headache and edema. Dose-related adverse reactions occurring in 1% of patients were as follows: edema, dizziness, hot flashes, and palpitations. Adverse reactions with unclear dose relationships but occurring in more than 1.0% of patients were as follows: headache, fatigue, nausea, abdominal pain, and somnolence. Among these adverse reactions, edema, hot flashes, palpitations, and somnolence were more common in women than in men. The following adverse events occurred at a rate (1% but 0.1% for which a causal relationship to the drug is unclear): General: allergic reaction, asthenia, back pain, hot flashes, malaise, pain, stiffness, weight gain; Cardiovascular: arrhythmia (including tachycardia, bradycardia, or atrial fibrillation), chest pain, hypotension, peripheral ischemia, syncope, postural dizziness, postural hypotension, and vasculitis; Central and Peripheral Nervous System: hypoesthesia, peripheral neuropathy, paresthesia, tremor, vertigo; Gastrointestinal: anorexia, constipation, dyspepsia , dysphagia, diarrhea, flatulence, pancreatitis, vomiting, gingival hyperplasia; musculoskeletal system: arthralgia, arthritis, muscle cramps, myalgia;Psychiatric system: sexual dysfunction, insomnia, tension, depression, nightmares, anxiety, depersonalization; Skin and appendages: angioedema, erythema, pruritus, rash, maculopapular rash; Special senses: visual disturbances, conjunctivitis, diplopia, eye pain, tinnitus; Urinary system: frequent urination, dysuria, nocturia; Autonomic nervous system: dry mouth, night sweats; Metabolic and nutritional system: hyperglycemia, Thirst; Hematopoietic system: leukopenia, purpura, thrombocytopenia. The incidence of the following adverse events (0.1%): heart failure, irregular pulse, premature contractions, skin discoloration, urticaria, dry skin, dermatitis, alopecia, muscle weakness, twitching, ataxia, hypertonia, migraine, cold and clammy skin, apathy, agitation, amnesia, gastritis, increased appetite, loose stools, cough, rhinitis, dysuria, polyuria, parosmia, taste disturbances, visual dysregulation, dry eyes. Other rare reactions include Myocardial infarction and angina pectoris cannot be distinguished as drug effects or disease states. Routine laboratory tests showed no significant changes, including serum potassium, blood glucose, total triglycerides, total cholesterol, high-density lipoprotein (HDL), uric acid, blood urea nitrogen, or creatinine. Post-marketing, there have been occasional reports of gynecomastia in patients taking the drug, but the causal relationship with the drug is unclear. In some cases, jaundice and elevated liver enzymes (often accompanied by cholestasis and hepatitis) have been severe, requiring hospitalization.
[Contraindications]
Allergy to dihydropyridine calcium channel blockers.
[Drug Interactions]
Clinical studies have not demonstrated a difference in the response of the elderly compared to the younger population to this drug. However, given that the elderly often have impaired liver, kidney, and heart function, as well as other medical conditions and medications, the lower end of the initial dose range is generally used. Elderly individuals have reduced clearance of this drug, with the area under the curve (AUC) increasing by approximately 40%-60%, necessitating a lower initial dose.
[Precautions]
(1) Angina pectoris and/or myocardial infarction: rare. Patients with severe obstructive coronary artery disease may experience an increase in the frequency, duration, and/or severity of angina attacks, or may develop acute myocardial infarction when starting calcium channel antagonist treatment or increasing the dose. The mechanism is unknown. (2) Hypotension: Since this product gradually produces a vasodilatory effect, acute hypotension is generally rare after oral administration. However, caution should still be exercised when this product is used in combination with other peripheral vasodilators, especially for patients with severe aortic valve stenosis. (3) Patients with heart failure: Calcium channel blockers should be used with caution in patients with heart failure. (4) Patients with hepatic insufficiency: This product should be used with caution in patients with severe hepatic insufficiency. (5) Patients with renal failure: The starting dose for patients with renal failure can remain unchanged. (6) Discontinuation of β-blockers: This product has no protective effect against rebound symptoms caused by sudden discontinuation of β-blockers. Therefore, the discontinuation of β-blockers still requires gradual reduction of the dose. (7) This product can be used safely in patients with obstructive pulmonary disease, well-compensated heart failure, peripheral vascular disease, diabetes and lipid disorders.
[Use in Elderly Patients]
Clinical studies have not confirmed that the elderly respond differently to this drug than the young. However, considering that the elderly often have impaired liver, kidney and heart function, and are accompanied by other diseases and corresponding drug treatments, the lower limit of the dose range is generally used for initial use. The clearance rate of this product is reduced in the elderly, and the area under the drug-time curve (AUC) increases by about 40%-60%, so a lower initial dose is also required.
[Overdose]
Drug Overdose can cause excessive peripheral vasodilation, leading to hypotension and possible reflex tachycardia. Following an overdose, blood pressure monitoring is essential, along with cardiac and respiratory monitoring. If hypotension develops, supportive care should be implemented, including limb elevation and volume expansion as needed. If these measures are ineffective, administration of pressors (such as phenylephrine) may be considered, provided circulating blood volume and urine output permit. Intravenous calcium gluconate can help reverse the calcium antagonist effect. Because this drug is highly bound to plasma proteins, dialysis is ineffective.
[Pharmacology and Toxicology]
Amlodipine besylate is a dihydropyridine calcium antagonist (calcium ion antagonist or slow-channel blocker). Cardiac and smooth muscle contraction depends on the release of extracellular calcium ions through specific ion channels. This drug selectively inhibits the transmembrane entry of calcium ions into smooth muscle cells and cardiomyocytes, with a greater effect on smooth muscle than on myocardium. Its interaction with calcium channels is determined by the progressive rate of binding and dissociation from receptor sites, resulting in a gradual onset of pharmacological action. This drug is a peripheral arterial dilator that acts directly on vascular smooth muscle, reducing peripheral vascular resistance and thereby lowering blood pressure. At therapeutic doses, negative inotropic effects have been observed in vitro but not in whole animal studies. This drug does not affect plasma calcium concentrations. Fifteen randomized, double-blind, placebo-controlled clinical trials have confirmed its antihypertensive effects. A once-daily dose can lower supine and standing blood pressure in patients with mild to moderate hypertension for 24 hours, and long-term use does not cause changes in heart rate or plasma BP. Catecholamine levels significantly changed. The antihypertensive effect was stable, with little difference between peak and trough values. The antihypertensive effect was dose-dependent, and the magnitude of the reduction correlated with pre-treatment blood pressure. Patients with moderate hypertension (diastolic blood pressure 105-114 mmHg) showed greater efficacy than those with mild hypertension (diastolic blood pressure 90-104 mmHg). Normotensive individuals showed no significant effect after taking the drug. The diastolic blood pressure-lowering effect of this drug was similar in the elderly and young, while the systolic blood pressure-lowering effect was stronger in the elderly. The precise mechanism by which this drug relieves angina pectoris is unclear, but it may be that during exercise, this drug reduces cardiac work and the rate-blood pressure product by reducing peripheral resistance (afterload), thereby reducing myocardial oxygen demand and treating exertional angina pectoris. It also inhibits calcium ions, epinephrine, serotonin, and thromboxane A2. It treats spontaneous angina by relieving the coronary artery and arteriolar constriction caused by exercise, restoring blood supply to the ischemic area. Five of eight clinical trials showed that this product significantly prolonged the duration of exercise-induced exertional angina; some studies showed that this product prolonged the time it took for the ST segment to change by 1 mm and reduced the frequency of angina attacks. This effect is sustained and does not significantly affect blood pressure or heart rate. A clinical trial conducted in 50 patients with spontaneous angina showed that this product could reduce angina attacks by four per week (placebo reduced it by one per week). Resting and exercise hemodynamics in patients with normal cardiac function after taking this product were measured, and cardiac ejection fraction increased, but there was no significant effect on dP/dt or left ventricular end-diastolic pressure/volume. At therapeutic doses, this product alone can reduce the risk of angina attacks. It does not cause negative inotropic effects, even when used alone or in combination with beta-blockers. In a placebo-controlled study, 697 patients with NYHA class I/II heart failure showed no worsening of heart failure after 8-12 weeks of treatment, as measured by exercise tolerance, NYHA class, symptoms, or left ventricular ejection fraction. Another placebo-controlled, long-term survival trial randomized 1,153 patients with class III/V heart failure to conventional treatment with amlodipine or placebo. The results showed that all-cause mortality and cardiac morbidity were 39% in the amlodipine group and 42% in the placebo group. This drug does not affect sinus node function or atrioventricular conduction. No electrocardiographic abnormalities were observed in patients with hypertension or angina pectoris treated with this drug in combination with beta-blockers. This drug does not alter The electrocardiogram of patients with angina pectoris was altered, without worsening atrioventricular block. In hypertensive patients with normal renal function, the drug reduced renal vascular resistance and increased glomerular filtration rate and renal blood flow, but did not alter filtration fraction or urinary protein. Carcinogenicity, Mutagenicity, and Teratogenicity: Amlodipine was administered to rats and mice daily at doses of 0.5, 1.25, and 2.5 mg/kg for two years without confirmed carcinogenicity. The highest dose reached the maximum tolerated dose in mice, but not in rats (calculated based on the maximum recommended clinical dose of 10 mg per square meter). No drug-related mutagenicity was revealed at either the gene or chromosomal level. Amlodipine was administered to male rats 64 days before mating, and to female rats 14 days before mating, at a dose of 10 mg/g daily (8 times the recommended dose). The maximum recommended human dose (MRHD) does not affect reproductive capacity. Administration of amlodipine at 10 mg/kg (8 and 23 times the MRHD) to pregnant rats and rabbits during the period of primary organogenesis revealed no teratogenicity or other embryotoxic effects. However, administration of 10 mg/g of amlodipine to rats, beginning 14 days before mating and continuing throughout mating and gestation, resulted in a significant reduction in pup size (approximately 50%), a significant increase in intrauterine mortality (approximately 5-fold), and prolonged gestation and delivery. Toxicity: Single doses of amlodipine up to 40 mg/kg and 100 mg/kg, respectively, can cause lethality in mice and rats. Single doses of 4 mg/kg or higher in dogs cause significant peripheral vasodilation and hypotension.