Product Overview
[Drug Name]
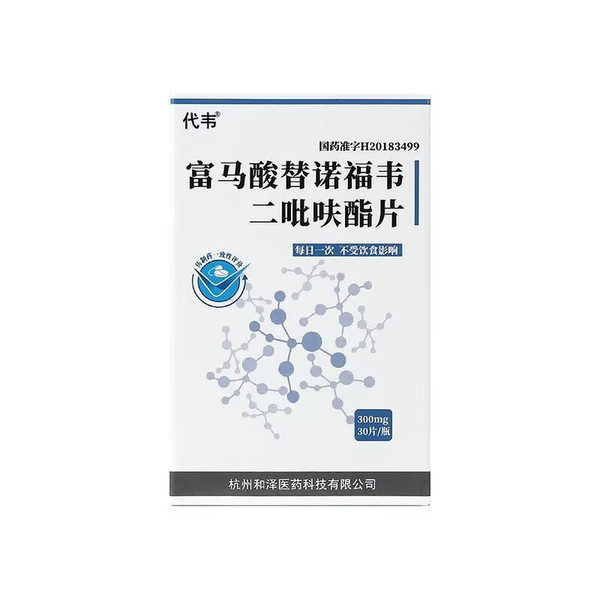
Generic Name: Tenofovir Disoproxil Fumarate Tablets
Trade Name: Daiwei Tenofovir Disoproxil Fumarate Tablets 300mg x 30 Tablets
[Main Ingredients]
Tenofovir Disoproxil Fumarate.
[Properties]
This product is a white or off-white film-coated tablet.
[Indications/Main Functions]
Indicated for use in combination with other antiretroviral drugs for the treatment of HIV-1 infection in adults and chronic hepatitis B in adults and children aged 12 years and older. See package insert for details.
[Specifications]
300mg x 30 tablets (Dawei)
[Dosage and Administration]
Take one tablet orally once daily, either on an empty stomach or with food.
[Adverse Reactions]
1. Lactic acidosis/toxic hepatomegaly with steatosis
2. Worsening of hepatitis B after treatment interruption
3. New onset or worsening renal impairment
4. Decreased bone mineral density
5. Immune reconstitution syndrome (see package insert for details)
[Contraindications]
Tenofovir disoproxil fumarate is contraindicated in patients with a prior hypersensitivity to any of the components of this drug.
[Drug Interactions]
1. This drug may interfere with the plasma concentration of didanosine. Tenofovir should be taken 2 hours before or 1 hour after didanosine.
2. Coadministration of didanosine with this drug may increase the plasma concentration of didanosine, increasing the risk of pancreatitis.
3. This drug is excreted from the kidneys via glomerular filtration and tubular secretion. Coadministration with other drugs excreted via tubular secretion may increase the plasma concentration of either drug. Drugs that reduce renal function may also increase the plasma concentration of this drug.
4. Concomitant use of this product with lamivudine, indinavir, lopinavir, and ritonavir may reduce the blood concentrations of these drugs. (See package insert for details.)
[Precautions]
Lactic Acidosis/Severe Hepatomegaly with Steatosis: Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with nucleoside analogs alone or in combination with other antiretroviral drugs. These cases mostly occurred in women. Obesity and chronic exposure to nucleosides may be risk factors. Special caution is advised when administering nucleoside analogs to patients with known risk factors for liver disease; however, cases have also been reported in patients without known risk factors. Tenofovir disoproxil fumarate treatment should be discontinued in any patient whose clinical or laboratory findings suggest lactic acidosis or significant hepatotoxicity (which may include hepatomegaly and steatosis, even in the absence of significant transaminase elevations). Hepatitis B worsens after treatment interruption. Patients infected with HBV who discontinue tenofovir disoproxil fumarate treatment must be closely monitored, including clinical and laboratory follow-up, for at least several months after discontinuation of treatment. If appropriate, patients may be allowed to resume anti-HBV treatment (see package insert for details).
[Pediatric Use]
In Study 115, 106 HBeAg-negative (9%) and positive (91%) subjects aged 12 to 18 years with chronic HBV infection were randomized to receive either tenofovir disoproxil fumarate 30 mg (N=52) or placebo (N=54) for 72 weeks of double-blind treatment. At study entry, the mean HBV DNA level was 8.1 log10 copies/mL and the mean ALT level was 101 U. Of the 52 subjects in the tenofovir disoproxil fumarate group, 20 were HBV-naïve/HBV-naïve, 3 were placebo-naïve, and 1 was placebo-naïve. 2 nucleoside/nucleic acid-experienced subjects. 31 of the 32 nucleoside/nucleic acid-experienced subjects had received lamivudine treatment. At week 72, 88% (46/52) of the subjects in the tenofovir disoproxil fumarate group and 0% (0/54) of the subjects in the placebo group achieved HBVDNA < 400 copies/mL. Among the subjects with abnormal ALT at baseline, 74% (26/35) of the subjects in the tenofovir disoproxil fumarate group had ALT normalization at week 72, while 31% (1342) of the subjects in the placebo group had ALT normalization at week 72. One subject in the tenofovir disoproxil fumarate group had persistent HBV infection during the first 72 weeks of the study. sAg negativity and anti-HBs seroconversion. The safety and efficacy of tenofovir disoproxil fumarate in children with chronic hepatitis B who are under 12 years of age or weigh less than 35 kg have not been established.
[Use in Elderly Patients]
Clinical trials of tenofovir disoproxil fumarate did not include sufficient numbers of subjects aged 65 years or older to determine whether their responses differ from those of younger subjects. In general, dose selection should be cautious in elderly patients, bearing in mind their increased risk of decreased liver, kidney, and heart function, concurrent illnesses, or ongoing medications.
[Overdose]
At doses higher than tenofovir disoproxil fumarate, the There is limited clinical experience with the therapeutic dose of tenofovir disoproxil fumarate 300 mg. In Study 901, eight subjects received 600 mg of oral tenofovir disoproxil fumarate for 28 days. No serious adverse reactions were reported. The possible effects of higher doses are unknown. If an overdose occurs, the patient must be monitored for evidence of toxicity and, if necessary, standard supportive care should be administered. Tenofovir is effectively removed by hemodialysis with an extraction coefficient of approximately 54%. Following a single dose of tenofovir disoproxil fumarate 300 mg, one 4-hour hemodialysis session will remove approximately the administered dose of tenofovir. 10% of the total.
[Pharmacology and Toxicology]
1. Pharmacology: Tenofovir disoproxil fumarate is a ring-opened nucleoside-activated diester analog of adenosine monophosphate. Tenofovir disoproxil fumarate is first converted to tenofovir through diester hydrolysis and then phosphorylated by cellular enzymes to form tenofovir diphosphate, also known as a chain terminator. Tenofovir diphosphate inhibits the activity of HCV-1 and HBV reverse transcriptases by competing with the natural substrate deoxyadenosine 5-triphosphate and terminating the DNA chain after integration into DNA. Tenofovir diphosphate is a weak inhibitor of mammalian DNA polymerases α and β, and mitochondrial DNA polymerase γ. Preparation. Toxicity: Tenofovir disoproxil fumarate can cause gene mutations in an in vitro mouse lymph test and was negative in an Ames test. In an in vivo mouse micronucleus test, the results of tenofovir disoproxil fumarate administration to male mice were negative. 2 Toxicology: Reproductive toxicity: Based on the comparison of body surface area, tenofovir disoproxil fumarate was administered to rats at a dose equivalent to 10 times that of humans. Male rats were given the drug for 28 consecutive days before mating, and female rats were given the drug for 15 consecutive days before mating to the 7th day of pregnancy. The results showed that tenofovir disoproxil fumarate had no effect on fertility, mating behavior and early embryonic development. See effects. However, changes in the estrous cycle occurred in female rats. Carcinogenicity: Long-term oral carcinogenicity studies of tenofovir disoproxil fumarate were conducted in mice and rats, with the highest exposure levels being approximately 16 times (mice) and 5 times (rats) the human therapeutic dose for HIV-1 infection, respectively. Female mice had an increase in hepatic adenomas at high doses (exposure levels 16 times higher than humans). No carcinogenicity was observed in rats at the highest exposure level of 5 times the human therapeutic dose. Other toxicities: In toxicology studies, rats, dogs, and monkeys were given tenofovir and tenofovir disoproxil fumarate at exposure levels greater than or equal to 6 times the human dose (based on AUC). Furoxetine has been associated with bone toxicity. In monkeys, bone toxicity was diagnosed as osteomalacia. In monkeys, osteomalacia was reversible after dose reduction or discontinuation of tenofovir.In rats and dogs, bone toxicity manifested as decreased bone mineral density. The underlying mechanism of bone toxicity is unknown, but evidence of renal toxicity was observed in four species. In these species, varying degrees of increase in serum creatinine, uric acid nitrogen, glycosuria, proteinuria, phosphaturia, and/or calciuria, as well as decreases in serum phosphate, were observed. These toxicities were observed at exposure levels 2-20 times higher than in humans (based on AUC). The relationship between renal abnormalities, particularly phosphaturia, and bone toxicity is unknown. (See package insert for details.)